While the emotional and psychological toll of post-traumatic stress disorder (PTSD) is widely recognized, many people are unaware of the physical effects it can have on those who have served in the armed forces. One of those effects is the often-overlooked link between PTSD and headache. By understanding this connection and recognizing the physical consequences that PTSD can take on the body, including PTSD headaches, we can better address the holistic well-being of those who have served our country.
What Is Post-Traumatic Stress Disorder?
PTSD is a mental health condition that some people develop after experiencing or witnessing a life-threatening event or something that elicited a feeling of fear, helplessness, or horror. It can lead to a range of symptoms, including:
- Flashbacks or nightmares
- Severe anxiety
- Emotional numbness
- Avoiding activities, places, or people associated with the event
- Insomnia
Given the nature of their service, Veterans are more likely to develop PTSD than civilians, and those who are deployed are more likely to have PTSD than Veterans who do not.1
Stress-Induced Tension Headaches
When someone with PTSD continuously experiences high levels of stress or anxiety, it can cause muscle tension, particularly around the neck and shoulders. This chronic muscle tension can lead to tension headaches, characterized by a dull, persistent pain that feels like a tight band around the head.
Sleep Disturbances
Another important factor in the PTSD-headache connection is sleep disturbances. Many Veterans with PTSD struggle with nightmares and insomnia, which can lead to a lack of restful sleep. Sleep is crucial for maintaining overall health, and when you’re not getting the rest your body needs, it can become more susceptible to various health issues, including headaches.
Think of it as a vicious cycle—PTSD leads to poor sleep, which in turn exacerbates headaches. One study found that half of patients who have tension headaches or migraines also have insomnia, and that poor sleep quality is very much associated with more frequent and severe headaches.2
Altered Brain Chemistry and Migraine
Brain scans in PTSD patients show a pattern of increased activity in certain parts of the brain, including the amygdala (the part that formulates your stress response), the hippocampus (where we store memories), and the medial prefrontal cortex (which deals with emotions and impulses).3
The constant and extreme state of stress, hyperarousal, and anxiety that many Veterans with PTSD experience can disrupt the brain’s delicate balance of neurotransmitters. Brain scans have shown that PTSD can cause chronic changes in specific regions of the brain, resulting in long-term changes to the brain’s “circuits” or the networks that connect the different regions of the brain.4 These chemical imbalances and changes have been known to trigger the onset of headaches, specifically migraines.
Managing PTSD-Related Migraine and Cluster Headache
Although Veterans and active-duty personnel are more likely to suffer from headache disorders than civilians,5 they don’t have to live with the pain.
If you’re a Veteran, the first step to understanding how to manage your headache pain better is to have a conversation with your VA health care provider, who can help you figure out the best treatment plan to suit your life. Fortunately, there are now options that don’t involve pills, injections, or drug-like side effects, like gammaCore™ non-invasive vagus nerve stimulator (nVNS).
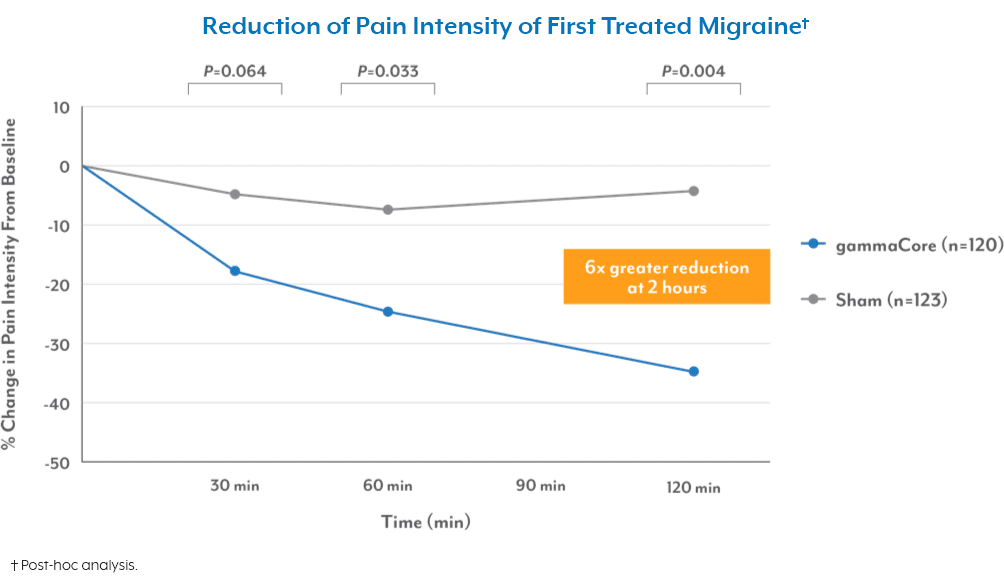
gammaCore nVNS is a portable, easy-to-use medical device with 6 FDA-cleared indications for migraine and cluster headache.6 With treatment sessions that take only 4 minutes, Veterans can use the device at home or while on the go to prevent headaches before they start or quickly stop painful attacks when they happen. gammaCore is available by prescription through your VA provider.
To see if gammaCore is right for you, call your VA health care provider or use the MyHealtheVet portal to schedule an appointment. Once prescribed by your VA provider, we’ll ship the device directly to your door. We can also follow up with personalized training to ensure you’re getting the most out of your treatments.
References
1. How Common is PTSD in Veterans? U.S. Department of Veterans Affairs. Retrieved October 26, 2023, from https://www.ptsd.va.gov/understand/common/common_veterans.asp
2. Fernández-de-las-Peñas, C., Fernández-Muñoz, J. J., Palacios-Ceña, M., et al. (2018). Sleep disturbances in tension-type headache and migraine. Therapeutic Advances in Neurological Disorders, 11. https://doi.org/10.1177/1756285617745444
3. The science and biology of PTSD. PTSD UK. Retrieved October 29, 2023, from https://www.ptsduk.org/what-is-ptsd/the-science-and-biology-of-ptsd/
4. The science and biology of PTSD. PTSD UK. Retrieved October 29, 2023, from https://www.ptsduk.org/what-is-ptsd/the-science-and-biology-of-ptsd/
5. (2017, May 22). Veterans who deployed are more likely to develop migraines or headache disorders. U.S. Department of Veterans Affairs. Retrieved October 29, 2023, from https://news.va.gov/38022/veterans-who-deployed-are-more-likely-to-develop-migraines-or-headache-disorders/
6. gammaCore Instructions for Use. (2023). elecroCore, Inc.