The unfortunate fact is that there is a higher incidence of migraine and cluster headaches among military Veterans, but the right information can help Veterans can get the upper hand on their headache attacks and stay in control. The American Migraine Foundation says that one-third of returning soldiers have migraine pain in the first month after coming home from the Middle East.1
The unfortunate fact is that there is a higher incidence of migraine and cluster headaches among military Veterans, but the right information can help Veterans can get the upper hand on their headache attacks and stay in control. The American Migraine Foundation says that one-third of returning soldiers have migraine pain in the first month after coming home from the Middle East.1
While Veterans get these type of headaches, studies repeatedly show they often times go undiagnosed. One reason may be the different conditions creating the migraines. For example, there are 414,000 Traumatic Brain Injuries (TBI) among servicemembers worldwide between 2000 and late 2019. More than 185,000 Veterans who use VA for their health care have been diagnosed with at least one TBI, and any form of headache is one of the most common symptoms after TBI.2
In the military, Veterans are taught to know their enemy. For military Veterans, the totality of impact from migraine or cluster headaches can go far beyond just the headache itself. Other effects include impairment through nausea, fogginess, pain, and side effects from drugs. And the layers of headache impact on Veterans can be physical, emotional, social/relational, and logistics/livelihood. Veterans need to understand the totality of these factors to be able to combat them effectively.
An important step to understanding how to better manage pain is Veterans having a conversation with a VA healthcare provider. A printable veteran headache discussion guide is a useful tool to help start the conversation with your healthcare team on what treatments may be right for you.
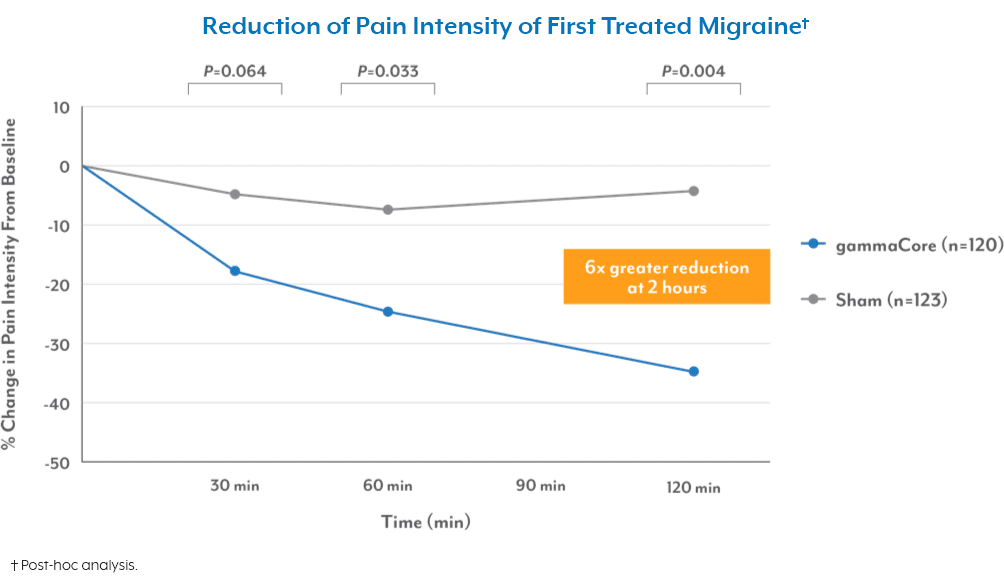
Once diagnosed, Veterans need to understand and discuss treatments with their healthcare provider to get the one that is right for them. Veterans may need treatments that are both preventative and acute for when attacks happen. Veterans should understand that treatments are no longer just pills and injections as they once were. Now there are other options. For example, the gammaCore SapphireTM 3 (nVNS) is a non-invasive vagus nerve stimulator. It is the first and only FDA-cleared therapy for the preventive treatment of migraine and cluster headache, and acute treatment of pain associated with migraine and episodic cluster headache.
Another important factor is matching treatment options to match the lifestyle of a military Veteran. For Veterans on the go, they need something that is portable, so if a migraine attack does occur, they know they can handle it. gammaCore Sapphire 3 fits in your pocket so you always have it on the go.
Unfortunately, headache effects are worsening under Covid. Migraines are up and stress is up. Nearly 70% of people with migraines report increase in attacks during Covid-193.
Because the pandemic can limit accessibility treatment options, Veterans need to stay up on the latest treatment options in these unusual times. Veterans need to know when home delivery is an option versus having to go into their provider for an injection or treatment. Also, Veterans should look for 1:1 virtual training and robust patient support programs if they are going to approach in-home treatments during Covid-19.
Veterans must self-advocate and work with their doctor to get the care best for them. Physicians are like anyone else and go with what they know. Veterans need to ask about different forms of treatments that best match to their type of headache and lifestyle. To find out more on the gammaCore Sapphire 3 visit https://gammacore.com/for-veterans/.
Please refer to the gammaCore Important Safety Information and Instructions for Use for all of the important warnings and precautions before using this product.
References
1. American Migraine Foundation website. https://americanmigrainefoundation.org/resource-library/post-traumatic-headache. Accessed October 29, 2019.
2. The Defense and Veterans Brain Injury Center (DVBIC), 2019.
3. 2020 Survey by Headache and Migraine Policy Forum and Migraine Again.