Migraine pain can be debilitating for anyone who experiences it. Still, for military Veterans, these headaches can be especially impairing due to their experiences and potential triggers. Understanding the unique aspects of migraine among Veterans and their possible causes is the first step in finding relief and managing pain.
Frequency of Migraine Among Military Veterans
If you’re a military Veteran who is struggling with migraine pain, know that you’re not alone. Veterans are more likely to suffer from migraine and other headache disorders than civilians.1
- More than a third of Veterans who served at least one year in Iraq or Afghanistan have been diagnosed with migraine or signs of migraine, according to the Department of Veterans Affairs.2
- Chronic migraine is believed to occur in around 3% of the population, compared to 20% or higher among post-9/11 combat Veterans, according to a 2020 article in the Journal of the American Association of Nurse Practitioners.3
- Although migraine is commonly treated in the Veteran’s Health Administration (VHA), there are likely more Veterans who do not seek health care or treatment for their migraine symptoms.4
Traumatic Brain Injury and Migraine
A traumatic brain injury (TBI) can be caused by a sudden or forceful bump, blow, or jolt to the head or body or from something that pierces the skull. Headache is the most frequently reported symptom after suffering a TBI, and headache pain can impact patients for several years after the injury.5
Veterans are at higher risk of experiencing a TBI because of their exposure to blasts, concussions, and head injuries inflicted during their military service. TBIs can disrupt normal brain function and lead to a variety of neurological and physiological changes, many of which can trigger painful headaches and increase the likelihood of developing migraines.
Mental Health and Migraine
Post-traumatic stress disorder (PTSD) is a mental health condition that develops after experiencing a traumatic or life-threatening event. PTSD affects at least 18% of combat Veterans but is believed to be underreported because of the stigma around mental health.6 Not only is the presence of PTSD associated with an increased predisposition to the development of migraine, but the odds of PTSD are increased in those with migraine.7
Given the connection between PTSD and migraine, it’s no surprise that migraine attacks are highly prevalent among Veterans with PTSD.
Another mental health concern among Veterans is depression. Although it may not garner as much attention as PTSD, it remains a prevalent issue in Veteran care. Contributing factors, such as separation from loved ones, stressors of combat, and witnessing oneself and others in harm’s way, can contribute to a higher risk of depression in both active-duty personnel and Veterans.8 Migraine and depression are directly connected—individuals who suffer from depression are 3.4 times more likely to develop migraine and migraine sufferers are almost 6 times more likely to suffer from depression.9
Managing Migraine Pain for Military Veterans
Coping with migraine symptoms is no easy feat, and if the pain is keeping you from living your life, it’s important that you seek professional help. There are many options that can offer relief, including medication, therapy, lifestyle changes, and support groups.
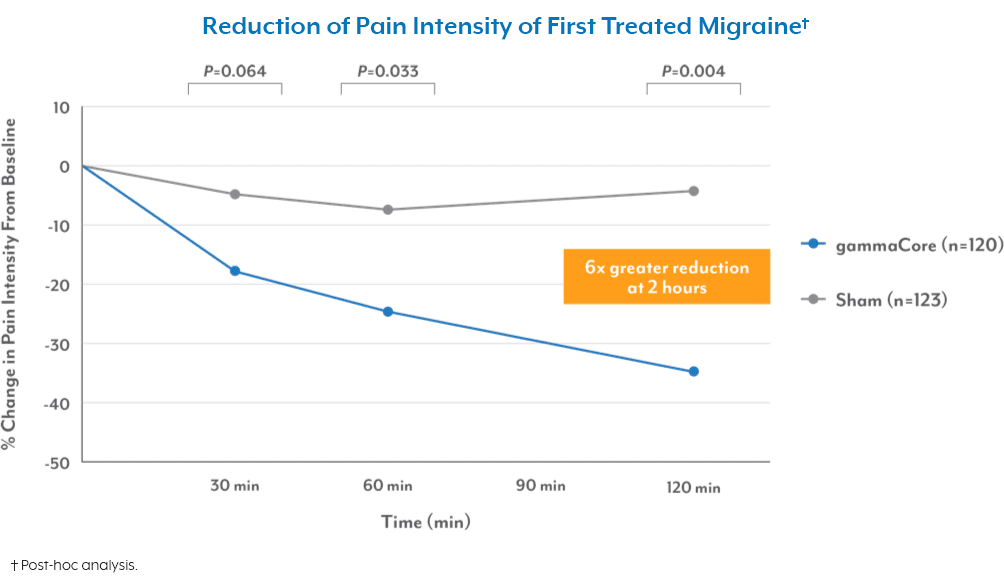
There’s also a non-surgical, non-drug treatment for migraine attacks that would be ideal for Veterans. gammaCore™ non-invasive vagus nerve stimulator (nVNS) is a small, handheld device that provides quick, easy treatments whenever and wherever you need it. You can use gammaCore nVNS twice daily for prevention (two 2-minute treatments) and up to 24 times daily to manage migraine pain as needed.
To see if gammaCore is right for you, call your VA health care provider or use the MyHealtheVet portal to schedule an appointment. Veterans who are not currently enrolled in the VA health care system may still qualify for migraine treatment through the VA. To apply, visit www.va.gov/healthbenefits/enroll or call 877-222-8387.
For more information about how gammaCore can help Veterans, contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. (2017, May 22). Veterans who deployed are more likely to develop migraines or headache disorders. U.S. Department of Veteran Affairs. Retrieved November 7, 2023, from https://news.va.gov/38022/veterans-who-deployed-are-more-likely-to-develop-migraines-or-headache-disorders/
2. (2017, May 22). Veterans who deployed are more likely to develop migraines or headache disorders. U.S. Department of Veteran Affairs. Retrieved November 7, 2023, from https://news.va.gov/38022/veterans-who-deployed-are-more-likely-to-develop-migraines-or-headache-disorders/
3. Williams, K. A. (2020). Headache management in a Veteran population: First considerations. Journal of the American Association of Nurse Practitioners, 32(11), 758-763. https://doi.org/10.1097/JXX.0000000000000539
4. Seng, E. K., Fenton, B. T., et al. (2022). Frequency, Demographics, Comorbidities, and Health Care Utilization by Veterans With Migraine. Neurology, 99(18). https://doi.org/10.1212/WNL.0000000000200888
5. Stacey, A., Lucas, S., et al. (2017). Natural History of Headache Five Years after Traumatic Brain Injury. Journal of Neurotrauma, 34(8), 1558-1564. https://doi.org/10.1089/neu.2016.4721
6. Nicole, L. R. (2014). Posttraumatic stress disorder in combat veterans. Journal of the American Academy of PAs, 27(5), 18-22. https://doi.org/10.1097/01.JAA.0000446228.62683.52
7. Petrarca, K. (2022, November 14). Migraine and Post Traumatic Stress Disorder. Association of Migraine Disorders. Retrieved November 28, 2023, from https://www.migrainedisorders.org/migraine-and-post-traumatic-stress-disorder/
8. Inoue, C., Shawler, E., et. al. (2023). Veteran and Military Mental Health Issues. StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/34283458/
9. (2022, February 22). The Relationship Between Migraines and Depression. Anxiety & Depression Association of America. Retrieved November 7, 2023, from https://adaa.org/webinar/consumer-professional/relationship-between-migraines-and-depression