 When we think of the brave men and women who serve in the military, we often picture them facing physical dangers on the battlefield. However, there’s another threat that many Veterans face, one that isn’t always immediately visible: traumatic brain injury (TBI). To put it simply, TBIs occur when a sudden trauma or blow to the head disrupts normal brain function. This disruption can range from mild to severe, depending on the extent of the injury.
When we think of the brave men and women who serve in the military, we often picture them facing physical dangers on the battlefield. However, there’s another threat that many Veterans face, one that isn’t always immediately visible: traumatic brain injury (TBI). To put it simply, TBIs occur when a sudden trauma or blow to the head disrupts normal brain function. This disruption can range from mild to severe, depending on the extent of the injury.
Why Is TBI a Relevant Issue Among Veterans?
For Veterans, the risk of sustaining a TBI is significantly higher due to the nature of military service and the various hazards that increase the likelihood of head injuries. Common causes of TBIs among Veterans include explosions, falls, or direct hits to the head during combat. Other activities like training exercises and vehicle accidents can also result in TBIs.
It’s estimated that up to 28% of service members have experienced a TBI.1 According to the U.S. Department of Veterans Affairs, over 185,000 Veterans who use the VA for health care are diagnosed with at least one TBI.2
What makes TBIs particularly concerning is their potential long-term impact on Veterans’ health and well-being. Apart from immediate symptoms like dizziness, confusion, and loss of consciousness, TBIs can lead to a host of chronic issues, including cognitive impairment, mood disorders, and, notably, headaches.
The TBI and Headache Connection
Headache is one of the most common persisting symptoms following a TBI.3 For Veterans specifically, there is also a connection between the number of TBIs a Veteran sustains and the severity and prevalence of headaches—Veterans with a history of two or more mild TBIs are more than twice as likely to experience severe headache symptoms and nearly six times more likely to experience migraine symptoms compared to Veterans with one mild TBI.4
TBI-induced headaches can vary in intensity and frequency, ranging from mild discomfort to severe migraines that significantly impair daily functioning. While the exact mechanisms underlying this link are not fully understood, several factors contribute to the development of headaches post-TBI, including:
- Brain Chemistry: TBIs can alter the brain’s chemical balance, affecting the neurotransmitters and hormones involved in pain regulation. This imbalance may contribute to the onset of headaches.
- Neurological Dysfunction: Damage to brain structures and pathways following a TBI can disrupt normal neurological processes. This leads to heightened sensitivity to pain signals and increased headache susceptibility.
- Musculoskeletal Issues: Injuries sustained during the traumatic event can cause tension and strain in the muscles and tissues surrounding the head and neck, triggering headaches as a secondary symptom.
- Psychological Factors: Coping with the aftermath of a TBI, including dealing with physical limitations and adjusting to changes in cognitive function, can induce stress and anxiety, both of which are known triggers for headaches.
How Veterans Can Reclaim Their Life After TBI
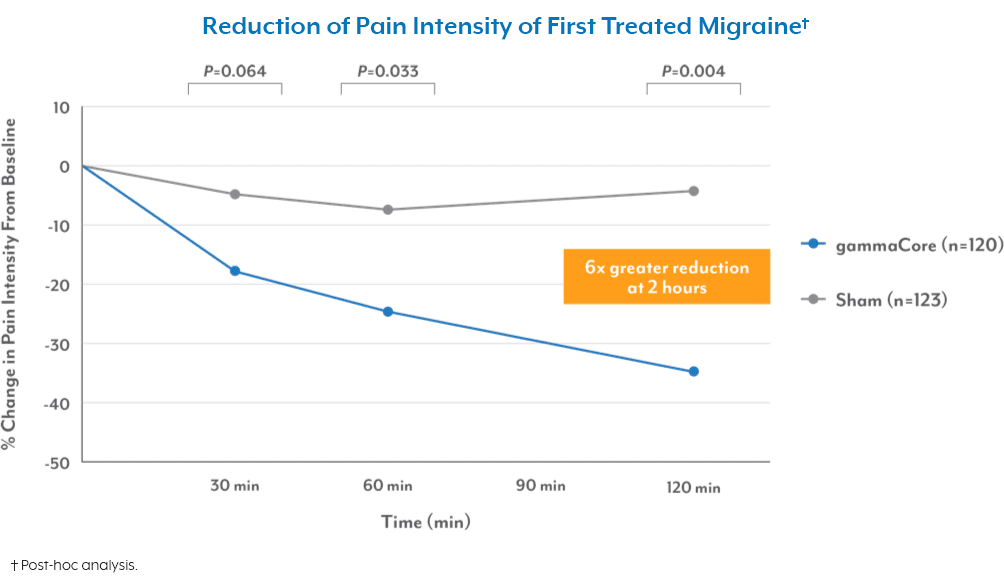
For Veterans struggling with TBI-related headaches, finding effective relief is crucial for improving their quality of life. One promising option is non-invasive vagus nerve stimulation (nVNS). This non-drug solution delivers mild electrical stimulation to the vagus nerve to intercept pain pathways in the brain, providing much-needed relief from painful headache symptoms.
gammaCore™ non-invasive vagus nerve stimulator (nVNS) is the first and only FDA-cleared non-invasive device to treat and prevent multiple types of headache pain via the vagus nerve. It’s small, handheld, and portable for quick and easy treatments whenever and wherever needed.
To see if gammaCore nVNS is right for you, call your VA health care provider or use the MyHealtheVet portal to schedule an appointment. Veterans who are not currently enrolled in the VA health care system may still qualify for migraine treatment through the VA. To apply, visit www.va.gov/healthbenefits/enroll or call 877-222-8387.
For more information about how gammaCore can help Veterans, contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. Reger, M. A., Brenner, L. A., & Du Pont, A. (2022). Traumatic Brain Injury and Veteran Mortality After the War in Afghanistan. JAMA Network Open, 5(2). https://doi.org/10.1001/jamanetworkopen.2021.48158
2. (n.d.). VA research on Traumatic Brain Injury (TBI). U.S. Department of Veterans Affairs. Retrieved March 4, 2024, from https://www.research.va.gov/topics/tbi.cfm
3. Hoffman, J. M., Lucas, S., et al. (2011). Natural History of Headache after Traumatic Brain Injury. Journal of Neurotrauma, 28(9), 1719–1725. https://doi.org/10.1089/neu.2011.1914
4. Coffman, C., Reyes, D., et al. (2022). Relationship Between Headache Characteristics and a Remote History of TBI in Veterans. Neurology, 99(2), e187–e198. https://doi.org/10.1212/WNL.0000000000200518