Migraines are more than just severe headaches; they often come with other symptoms that can significantly impact daily life. What many people may not realize is that there are also different types of migraine, including ocular migraine. As you may have guessed, this is a type of migraine that primarily affects vision, and it may also be referred to as a visual migraine or retinal migraine. Unlike other migraines, which primarily cause head pain, an ocular migraine is characterized by temporary visual disturbances. These disturbances can range from seeing flashes of light or zig-zag lines in vision with no headache to experiencing blind spots or even temporary vision loss in one eye (unlike migraine with aura, which affects both eyes). Understanding ocular migraine symptoms can help you identify and manage these episodes more effectively.
Migraines are more than just severe headaches; they often come with other symptoms that can significantly impact daily life. What many people may not realize is that there are also different types of migraine, including ocular migraine. As you may have guessed, this is a type of migraine that primarily affects vision, and it may also be referred to as a visual migraine or retinal migraine. Unlike other migraines, which primarily cause head pain, an ocular migraine is characterized by temporary visual disturbances. These disturbances can range from seeing flashes of light or zig-zag lines in vision with no headache to experiencing blind spots or even temporary vision loss in one eye (unlike migraine with aura, which affects both eyes). Understanding ocular migraine symptoms can help you identify and manage these episodes more effectively.
Common Symptoms
The most common symptoms of an ocular migraine include:
- Visual Disturbances: This can manifest as shimmering or flickering lights, zigzag lines, or blind spots.
- Partial or Complete Vision Loss: Some people may experience partial or complete vision loss in one eye, usually lasting less than an hour.
- Headache: Although headaches are not always present, some people might experience one following the visual disturbances.
It’s essential to note that the visual symptoms of an ocular migraine are temporary and usually resolve on their own within 20 to 30 minutes.
What Causes Ocular Migraine
The exact cause of ocular migraines remains unclear, but it may be related to reduced blood flow or blood vessel spasms around the retina or behind the eye.1 Studies have shown that almost a third of ocular migraine patients have a history of migraine, and 50% have a family history of migraine.2
Like traditional migraines, there are certain triggers that can lead to an ocular migraine episode, including stress, hormonal changes, particular foods or drinks (like caffeine or alcohol), dehydration, and bright or flickering lights. Other precipitating factors for ocular migraine may include hypertension (high blood pressure), hypoglycemia (low blood sugar), and hyperthermia (excessive heat).3
Managing Ocular Migraine?
While there’s no cure, several strategies can help manage and reduce the frequency of episodes:
- Identify and Avoid Triggers: Keeping a migraine diary can help identify triggers, enabling you to make the necessary lifestyle changes to avoid them.
- Stay Hydrated: Drinking plenty of water throughout the day can help prevent dehydration, a common migraine trigger.
- Manage Stress: Practicing relaxation techniques like deep breathing, meditation, or yoga can help reduce stress levels.
- Medication: Over-the-counter pain relievers or prescription medications may help alleviate migraine symptoms. Always consult with a health care professional before starting any medication.
Ocular migraines can be scary and disorienting, especially if you don’t know what’s happening. That’s why if you suspect you’re experiencing an ocular migraine, it’s crucial to consult with a health care professional for an accurate diagnosis.
Your health care provider will also be able to recommend the right treatment plan for your migraine attacks. While traditional medications can be effective for some people, others may be looking for alternative solutions for migraine relief. This is where gammaCore™ non-invasive vagus nerve stimulator (nvNS) comes in.
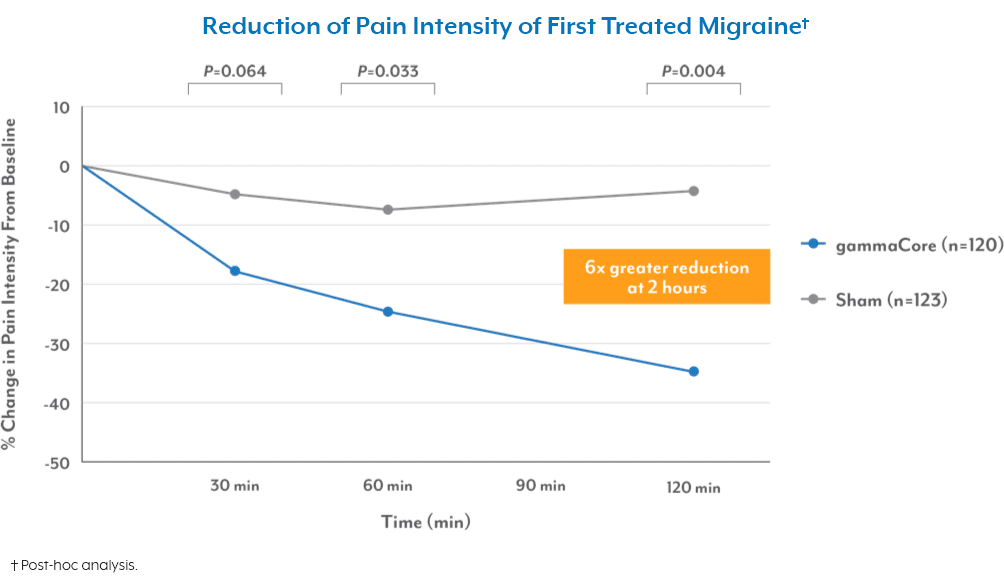
gammaCore nVNS is a non-drug, FDA-cleared device designed to treat and prevent multiple types of headache pain, including ocular migraine, by using gentle electrical stimulation to target the vagus nerve (which plays a key role in regulating pain). The best part is that gammaCore can be used twice daily to prevent migraine attacks or at the onset of symptoms, making it a convenient and portable solution for relief anytime, anywhere. Plus, it’s free from the side effects often associated with medications, making it a safe and well-tolerated option for many migraine sufferers.
To see if gammaCore is right for you, visit our clinic finder to locate a health care provider near you, or contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. (n.d.). Ocular Migraine. American Optometric Association. Retrieved March 27, 2024, from https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/ocular-migraine?sso=y
2. Pradhan, S., & Chung, S. M. (2004). Retinal, ophthalmic, or ocular migraine. Current Neurology and Neuroscience Reports, 4(5), 391-397. https://doi.org/10.1007/s11910-004-0086-5
3. Khalili, Y. A., Jain, S., & King, K. C. (2024). Retinal Migraine Headache. StatPearls Publishing.