As the chill of winter fades away, many people eagerly welcome the arrival of spring with the longer days and warmer temperatures. However, for migraine sufferers, the change in season brings with it a host of triggers that can lead to debilitating headaches. Here are some of the most common migraine triggers to watch out for this spring, plus steps you can take to manage them so that you can get out and enjoy all that the season has to offer.
Top Spring Migraine Triggers
- Weather Changes
Spring is notorious for its fluctuating weather patterns, with sudden shifts in temperature, humidity, and barometric pressure. These changes can disrupt the delicate balance of brain chemicals and blood vessels, which can wreak havoc for migraine-prone individuals. Barometric pressure, in particular, plays a crucial role in triggering migraines. When barometric pressure drops rapidly, as often happens during spring storms or sudden temperature changes, it can cause blood vessels in the brain to dilate and trigger migraine attacks. Similarly, high humidity levels have been shown to increase the likelihood of migraines.1
How to Manage It: Keep an eye on upcoming weather patterns and plan accordingly. By monitoring weather forecasts, you can anticipate days when your migraine risk may be higher and take steps to mitigate potential triggers. For example, if you know a storm is approaching, try to rest and relax indoors, stay hydrated, and avoid exposure to extreme temperatures or sudden weather changes.
- Allergens
While the blooming flowers and trees are a pleasant sight for many, the fresh greenery also means more pollen in the air, triggering allergies for many people. Allergic reactions can often trigger migraines in susceptible individuals. When you’re exposed to allergens, your immune system releases certain chemicals that can fuel inflammation in the body, the perfect storm for a migraine attack.
How to Manage It: Keep windows closed during high-pollen days, use air purifiers indoors, and consider wearing a mask when spending time outdoors to reduce exposure to allergens.
- Bright Light
Longer days and more sunlight in the spring also mean more bright light, which is another common migraine trigger. The mechanism behind light-induced migraines is complex and not entirely understood, but it’s believed that certain wavelengths of light can disrupt the brain’s neurochemistry, leading to migraine attacks in susceptible individuals.
How to Manage It: Wear polarized sunglasses with UV protection outdoors, especially on sunny days, and choose a style with large frames or wraparound designs for maximum coverage. In addition, consider using tinted screens or filters and adjust brightness settings on electronic devices to reduce glare and alleviate eye strain. It would also be helpful to have blackout window coverings and dimmer switches at home to create a more comfortable lighting environment when you need it.
- Irregular Sleep Patterns and Changes in Routine
Whether it’s spring cleaning, gardening, or spending more time outside, the change in season often brings about changes in routine. While these activities can be enjoyable, they can also disrupt sleep patterns and throw your routine off kilter, which, as you may have guessed, can trigger uncomfortable migraines for some individuals.
How to Manage It: Try to maintain a consistent sleep schedule, even on weekends, and create a relaxing bedtime routine to help you wind down at night. If you’re trying new activities this spring, pace yourself and listen to your body’s signals for rest.
Getting Ahead of Spring Migraines
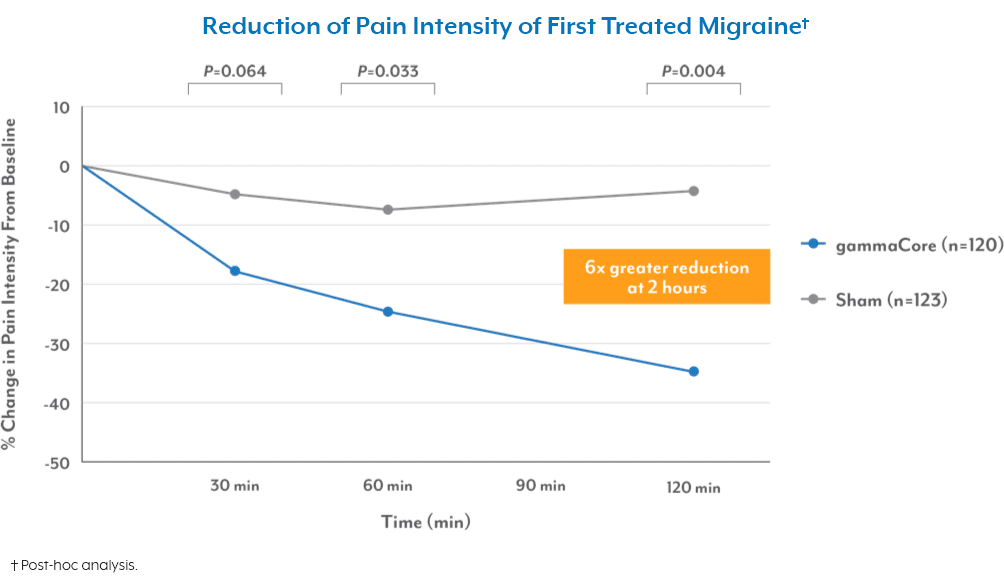
Despite your best efforts to avoid the triggers this spring, staying prepared is essential if an unexpected migraine strikes. One way to ensure you’re always a step ahead is by keeping gammaCore™ non-invasive vagus nerve stimulator (nVNS) on hand. This portable, handheld device, available with a prescription from your health care provider, is FDA-cleared to treat migraines as needed and prevent future attacks with just two 2-minute stimulations twice daily.
To see if gammaCore is right for you, visit our clinic finder to locate a health care provider near you, or contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. Elcik, C., Fuhrmann, C. M., Mercer, A. E., et al. (2017). Relationship between air mass type and emergency department visits for migraine headache across the Triangle region of North Carolina. International Journal of Biometeorology, 61(12), 2245-2254. https://doi.org/10.1007/s00484-017-1432-z