As if periods weren’t enough of a rollercoaster ride, some women also have to deal with the added punch of menstrual migraine, also known as hormonal migraine or PMS headache. These intense headaches add an extra layer of distress to what can already be an uncomfortable time of the month for a lot of women. As many as 70% of women who struggle with migraines have noticed a connection between their period and their migraine attacks.1 Understanding the connection between migraine and your monthly cycle will make it easier to not only manage the pain but also help prevent future attacks.
What Is Menstrual Migraine?
Menstrual migraine is a specific type of headache that typically occurs in association with a woman’s menstrual cycle. Unlike a regular migraine, which can strike at any time, menstrual migraines are more predictable—they usually happen in the days leading up to menstruation (around two days before) and continue through the first couple of days of a menstrual period. For many women, a menstrual migraine tends to be longer, more severe, and cause more light sensitivity than migraine attacks during other times of the month.2
The Link Between Menstruation and Migraine
Researchers believe that hormonal fluctuations play a crucial role in the connection between menstruation and migraine. The two main hormones involved are estrogen and progesterone, which naturally rise and fall during the menstrual cycle.
Estrogen levels start rising in the days before ovulation, reaching their peak just before menstruation. For some women, this increase in estrogen can trigger changes in the brain that can lead to a pre-menstrual migraine. After ovulation and as menstruation begins, estrogen levels drop sharply while progesterone levels surge. The sensitivity of the brain to these hormonal changes may explain why some women are more prone to migraines during specific phases of their menstrual cycle.3
Managing Menstrual Migraine
If you struggle with menstrual migraine, your life doesn’t need to come to a standstill every month. There are ways to effectively manage and reduce the impact of these headaches so you can get back to doing the things you love.
- Tracking Your Cycle: Keep a diary to track your cycle and note when migraines occur. There are also many apps available that can help you document dates, symptoms, and more. These details help you identify patterns and anticipate when you are most susceptible to a menstrual migraine attack. Keeping track of your menstrual cycle will also help your health care provider diagnose and provide better guidance for your menstrual migraine treatment.
- Hormonal Contraceptives: For some women, hormonal contraceptives can help regulate hormonal fluctuations and reduce the occurrence of menstrual migraine. Consult with your health care provider to determine if this might be a suitable option for you.
- Lifestyle Changes: A healthy lifestyle that includes regular exercise, sufficient sleep, and a balanced diet will contribute to overall well-being and may help reduce the frequency and severity of migraines. Calming relaxation techniques like deep breathing, meditation, or yoga may also provide relief by keeping your stress levels in check.
- Over-the-counter Pain Relief: Over-the-counter pain medications, such as nonsteroidal anti-inflammatory medications (NSAIDs), can help alleviate the symptoms of a migraine. These should ideally be taken two or three days before a period starts and continued through your cycle to keep migraine pain at bay.
- Magnesium: Magnesium supplements taken orally or intravenously have been shown in a clinical trial to help prevent menstrual migraine.4 The best way to use magnesium is to take it 15 days after your period starts and continue until the next cycle begins. This treatment can work for women with irregular cycles because the time is based on your previous period.5 Finding the correct dose is essential with this treatment to avoid the most frequent side effects of diarrhea and abdominal cramping.6
- Vagus Nerve Stimulation: Non-invasive vagus nerve stimulation (nVNS) is proven to be a safe and tolerable preventative menstrual migraine treatment that can reduce the number of headache days. It also works to relieve menstrual migraine pain.7
gammaCore™ nVNS is a portable, handheld device you can use in the comfort of home to manage menstrual migraine pain. It’s clinically proven to prevent migraines when used twice daily and provide fast-acting pain relief when you need it. The best part is that treatment sessions with gammaCore take less than five minutes, so you can be up and moving before you know it.
3 Reasons to Choose gammaCore for Your Menstrual Migraine Pain
It’s a safe, reliable non-drug solution for menstrual migraine pain. gammaCore is designed to provide migraine relief for women when they need it most and doesn’t require the use of any additional medications8, so you won’t have to worry about drug-related side effects. gammaCore is also clinically tested to be safe and tolerable.9
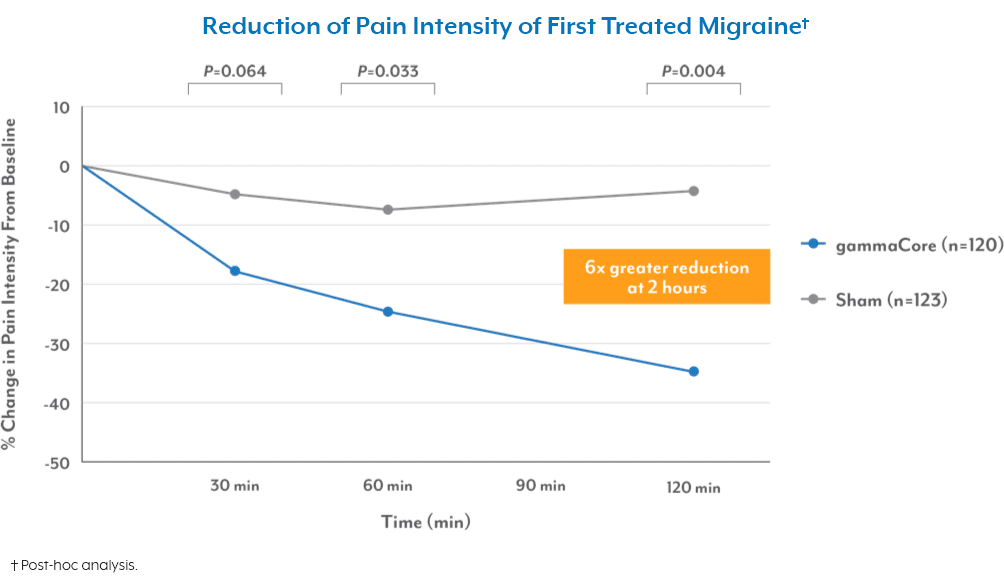
It gets to work fast. gammaCore has been shown to relieve migraine pain in as little as 30 minutes after treatment.10
It’s proven to deliver lasting results. The evidence speaks for itself. One study found that using gammaCore significantly reduced the average number of menstrual-related migraine days by 35%—nearly 40% of patients experienced a reduction of more than half. For migraines that did occur, treatment with gammaCore resulted in less intense attacks and reduced the need for pain medication by 37%.11
To see if gammaCore is right for you, visit our clinic finder to locate a health care provider near you, or contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. Silberstein, S. D. (1996). Menstrual migraine. Journal of Women’s Health & Gender-Based Medicine, 8(7), 919-31. https://doi.org/10.1089/jwh.1.1999.8.919
2. (2021, November 5). Menstrual Migraine Treatment and Prevention. American Migraine Foundation. Retrieved January 15, 2024, from https://americanmigrainefoundation.org/resource-library/menstrual-migraine-treatment-and-prevention/
3. Reddy, N., Desai, M. N., Schoenbrunner, A., et al. (2021). The complex relationship between estrogen and migraines: A scoping review. Systematic Reviews. https://doi.org/10.1186/s13643-021-01618-4
4. Facchinetti, F., Sances, G., Borella, P., et al. (1988). Magnesium prophylaxis of menstrual migraine: Effects on intracellular magnesium. Headache, 31(5), 298-301. https://doi.org/10.1111/j.1526-4610.1991.hed3105298.x
5. (2021, November 5). Menstrual Migraine Treatment and Prevention. American Migraine Foundation. Retrieved January 15, 2024, from https://americanmigrainefoundation.org/resource-library/menstrual-migraine-treatment-and-prevention/
6. (2021, October 20). Magnesium and Migraine. American Migraine Foundation. Retrieved January 16, 2024, from https://americanmigrainefoundation.org/resource-library/magnesium/
7. Grazzi, L., Egeo, G., Calhoun, A. H., et al. (2016). Non-invasive Vagus Nerve Stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migraine: An open-label study. The Journal of Headache and Pain, 17. https://doi.org/10.1186/s10194-016-0684-z
8. Grazzi, L., Egeo, G., Calhoun, A. H., et al. (2016). Non-invasive Vagus Nerve Stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migraine: An open-label study. The Journal of Headache and Pain, 17. https://doi.org/10.1186/s10194-016-0684-z
9. Ben-Menachem, E., Revesz, D., Simon, B. J., & Silberstein, S. D. (2015). Surgically implanted and non‐invasive vagus nerve stimulation: a review of efficacy, safety and tolerability. European Journal of Neurology, 22(9), 1260–1268. https://doi.org/10.1111/ene.12629
10. Tassorelli, C., Grazzi, L., De Tommaso, M., Pierangeli, G., Martelletti, P., Rainero, I., Dorlas, S., Geppetti, P., Ambrosini, A., Sarchielli, P., Liebler, E., & Barbanti, P. (2018c). Noninvasive vagus nerve stimulation as acute therapy for migraine: The randomized PRESTO study. Neurology, 91(4), e364–e373. https://doi.org/10.1212/wnl.0000000000005857
11. Grazzi, L., Egeo, G., Calhoun, A. H., et al. (2016). Non-invasive Vagus Nerve Stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migraine: An open-label study. The Journal of Headache and Pain, 17. https://doi.org/10.1186/s10194-016-0684-z